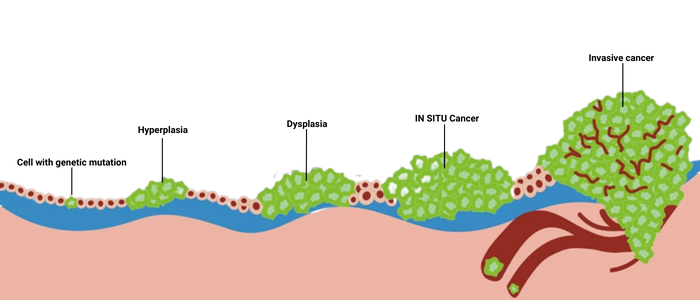
In a healthy person, body cells grow and multiply to replace old or damaged cells.
However, when the abnormal or damaged cells continue to grow and multiply, they form abnormal clumps of tissue called tumours, which can be cancerous (malignant) or noncancerous (benign).
Cancerous cells disrupt the normal function and affect the behaviour of the normal cells, molecules and blood vessels near the tumour. With this, it can easily lead to the growth of tumours and the spreading of cancerous cells to the surrounding tissues, then migrating (metastasize) to distant parts of the body to form more tumours.
In certain cases, some patients may remain asymptomatic or may neglect the early signs and symptoms of cancer.
In fact, delay in detection provides the opportunity for cancer to spread without any medical intervention. By the time the patient seeks medical help, chances are that it may be already too late to treat or recover.
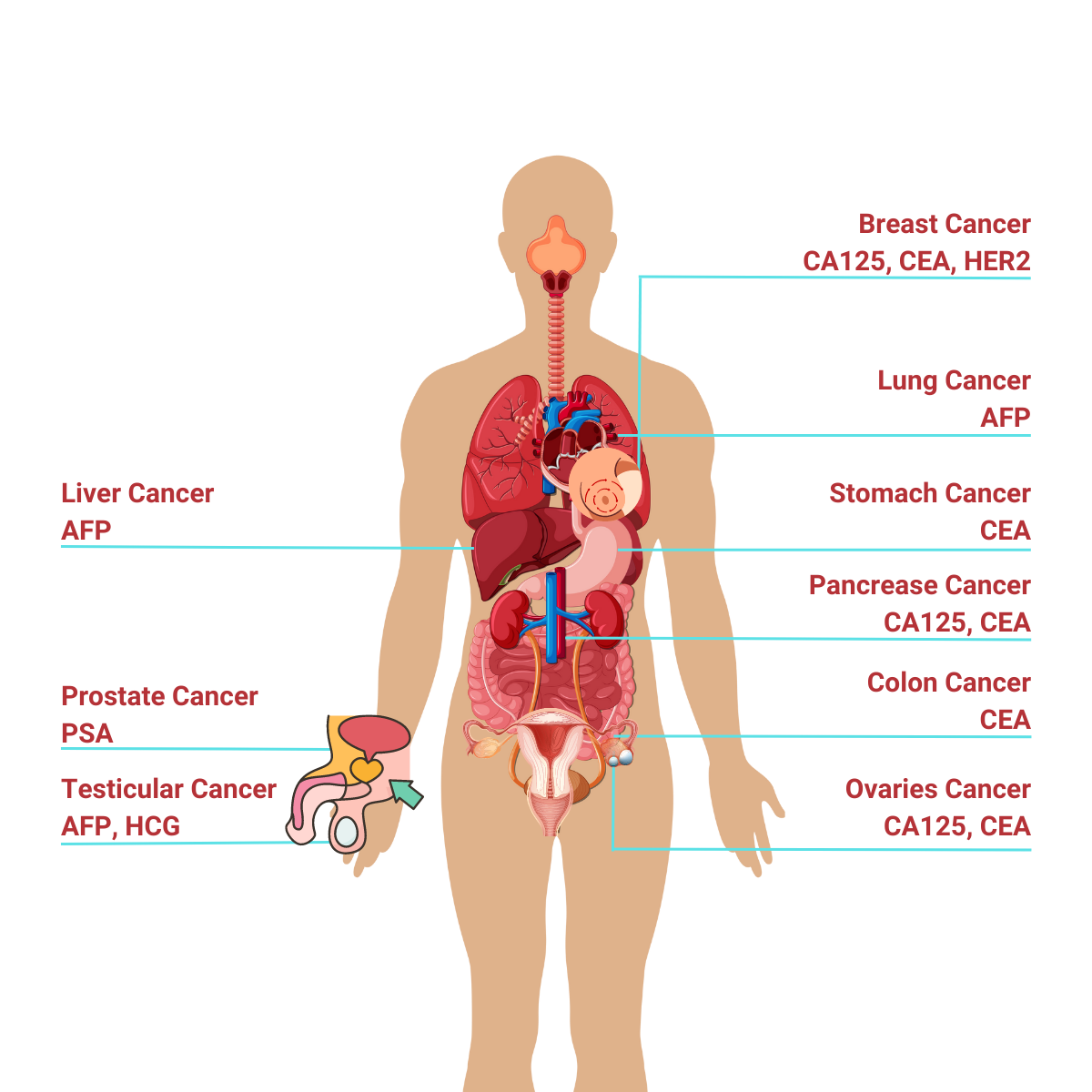
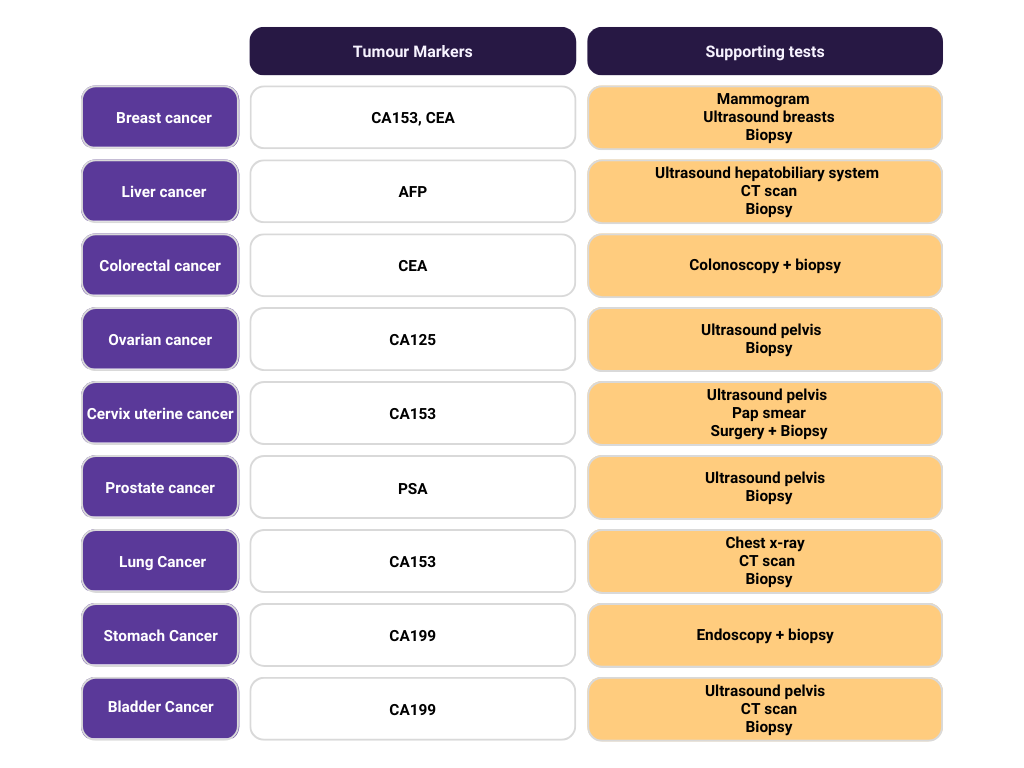
Clinical application of tumour markers can be broadly classified into 4 groups: Screening and early detection, diagnostic confirmation, prognosis and prediction of therapeutic response and monitoring disease and recurrence.
Indeed, tumour markers by cells include a variety of substances like cell surface antigens, cytoplasmic proteins, enzymes, hormones, oncofetal antigens, receptors, oncogenes and their products. It is usually produced by the cancer cells or other cells in the body in response to the presence of cancer.
In Malaysia, there are five most common cancers which are:
Life Care Diagnostic Medical Centre Sdn. Bhd. 200401034597 (673106-V)
Bangsar South
WhatsApp: 0122343610
1st Floor, Wisma Lifecare,
No. 5, Jalan Kerinchi, Bangsar South,
59200 Kuala Lumpur
Cheras South
WhatsApp: 01127213620
19A-2 & 19B-2, Block E, Kompleks Komersil Akasa,
Jalan Akasa, Akasa Cheras Selatan,
43300 Seri Kembangan, Selangor
Operating Hour:
Monday – Friday: 8.00am – 5.00pm
Saturday: 8.00am – 1.00pm
Sunday & Public Holidays: Closed

Drop us your email to know more about our monthly deals and health tips!